Even though my last post was quite extensive in detail, there is still more to talk about! But before I get into that, I have to introduce two new faces: Max and Tatum (both undergrad students). Now, unlike my previous posts, I cannot go into extensive details due many of the methods and details being proprietary.
As I mentioned last time, the electrospinner creates scaffolds. These scaffolds can then be placed in a wound in order to accelerate healing. But, there's one problem: pathogens. While the wound heals, the site needs to be protected from deadly bacteria (pathogens) that could potentially impair wound healing. So the question is how to protect the wound?
This leads us to Max and Tatum. One of the ideas that they are exploring is the combination of scaffolds with an antimicrobial therapeutic. So what exactly does this mean? In order for this to make sense, you have to remember how electrospinning works: we use a gelatin to create the scaffolds. The gelatin mixture is pumped from the syringe and sprayed onto the target, ultimately making a scaffold. Now, since we can modify what we put in the syringe, we can modify the properties of the scaffold. In this case, if we add an antimicrobial therapeutic to the gelatin in the syringe, we can create a scaffold resistant to harmful bacteria.
Now that's pretty cool.
At the moment, we are still experimenting with how much of the therapeutic we should add to the scaffold. Too much, and it might be a waste. Too little, and bacteria might still grow. So this is why we spin multiple scaffolds, each with different amounts of added therapeutic. But here's the catch, each scaffold takes an hour to spin. Let's just say, lots of music was listened to while waiting...
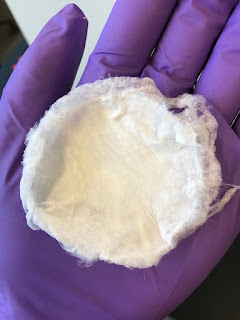
The end result:
As you can see, nothing looks out of the ordinary; it's just another scaffold. But inside, it has a secret weapon: antimicrobial therapeutics. Pathogens beware!
Now that the scaffolds are all set and done, we have to test them. Each scaffold will be placed into a dish with growing bacteria. Depending on the results, we may be one step closer to creating a pathogen-resistant scaffold.
-Tudor